The best management approach for hypertension involves a combination of nonpharmacological and pharmacological interventions.

The American College of Cardiology (ACC) and the American Heart Association (AHA) recommend the
following nonpharmacological interventions as first-line strategies for all patients with hypertension:
1. Weight loss: Achieving and maintaining a healthy weight can significantly reduce blood pressure.
2. DASH diet: The Dietary Approaches to Stop Hypertension (DASH) diet emphasizes fruits, vegetables,
whole grains, and low-fat dairy products while reducing saturated fat and cholesterol intake.
3. Sodium reduction: Limiting sodium intake to less than 2,300 mg per day, with an ideal goal of less
than 1,500 mg per day for most adults.
4. Potassium supplementation: Increasing dietary potassium intake to 3,500-5,000 mg per day,
preferably through food sources.
5. Physical activity: Engaging in regular aerobic physical activity, such as 90-150 minutes per week of
moderate-intensity exercise.
6. Alcohol reduction: Limiting alcohol intake to no more than two drinks per day for men and one drink
per day for women.[1]
What means stage 1 or stage 2 Hypertension category?
Stage 1 defines the top number of blood pressure between 130 and 139 mm Hg or the bottom number is between 80 and 89 mm Hg
Stage 2 defines the top number of blood pressure between 140 mm Hg or higher or the bottom number is between 90 mm Hg or higher
For patients with stage 1 hypertension who do not achieve target blood pressure with lifestyle
modifications alone, or for those with stage 2 hypertension, pharmacological treatment is
recommended. Initial drug therapy typically includes:
1. Thiazide diuretics
2. ACE inhibitors or ARBs
3. Calcium channel blockers
The choice of initial medication should be based on individual patient characteristics, comorbid
conditions, and potential drug interactions.[1]
what if I do not target my blood pressure target?
For patients who do not achieve target blood pressure with monotherapy, combination therapy with
two or more antihypertensive agents may be necessary. Regular monitoring and follow-up are essential
to ensure treatment efficacy and adherence.[1]
The management of hypertension should be tailored to the individual patient, considering both
nonpharmacological and pharmacological strategies.

Recommendations for patients stage 1 and 2
For patients with stage 1 hypertension without cardiovascular disease, diabetes mellitus, or chronic
kidney disease, the 2017 ACC/AHA guidelines recommend calculating the 10-year risk of atherosclerotic
cardiovascular disease (ASCVD). If the risk is less than 10%, lifestyle modifications alone may be
sufficient for 3 to 6 months. These modifications include dietary sodium restriction, weight loss, regular
physical activity, moderation of alcohol intake, and increased consumption of potassium-rich foods.[2]
For patients with stage 2 hypertension or those with a 10-year ASCVD risk of 10% or higher,
pharmacological treatment should be initiated alongside lifestyle changes. The initial antihypertensive
agent should be selected from one of four drug classes: ACE inhibitors, angiotensin receptor blockers
(ARBs), calcium channel blockers, and thiazide-type diuretics. The choice of agent should be guided by
the patient's clinical characteristics, coexisting conditions, and potential side effects.[2]
What medical evidence recommends ?
The SPRINT trial supports a lower systolic blood pressure target of less than 120 mm Hg, which has been
associated with reduced hypertension-related morbidity and all-cause mortality. However, this target
may increase the risk of electrolyte abnormalities, syncope, and acute kidney injury, particularly in older
adults.[2]
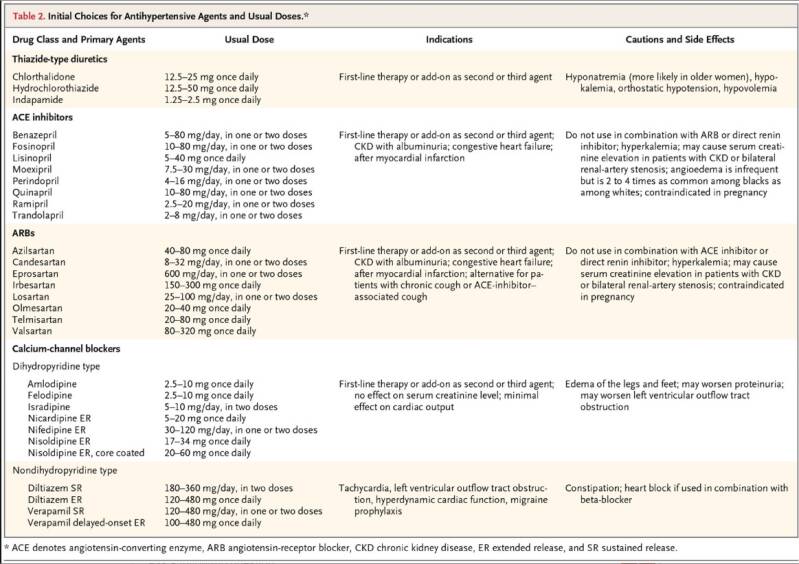
Table 2. Initial Choices for Antihypertensive Agents and Usual Doses.*
Initial Treatment of Hypertension. N Engl J Med. February 14, 2018.
This table provides a comprehensive overview of the initial choices for antihypertensive agents,
including usual doses, indications, and potential side effects. It is essential to consider patient-specific
factors such as age, race, and comorbidities when selecting the most appropriate antihypertensive
therapy. Regular follow-up and monitoring are crucial to ensure effective blood pressure control and to
adjust treatment as needed.
By Dr. Nanna
References
1. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the
Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report
of the American College of Cardiology/American Heart Association Task Force on Clinical
Practice Guidelines.Whelton PK, Carey RM, Aronow WS, et al. Circulation. 2018;138(17):e484-
e594. doi:10.1161/CIR.0000000000000596.
2. Initial Treatment of Hypertension. Taler SJ. The New England Journal of Medicine.
2018;378(7):636-644. doi:10.1056/NEJMcp1613481.


Add comment
Comments